Protecting patients and staff from acquiring SARS-CoV-2 in hospitals during the COVID-19 pandemic has proven challenging. The United Kingdom experienced two severe waves of COVID-19 in 2020 with some of the highest mortality rates in Europe. During periods of high case rates, hospitals were a particular concern for SARS-CoV-2 exposure of vulnerable patients. As rates of SARS-CoV-2 in the community increased, so did cases of SARS-CoV-2 acquired within the hospital.
Hospital acquired COVID-19 infections are a serious problem because they lead to high mortality rates in vulnerable patients, interruption of routine care, closure of ward areas, and staff shortages due to infection of healthcare workers. Infection control practice aims to prevent hospital-acquired infections through prompt isolation of infectious patients, identification of contacts and interruption of modes of transmission. Unfortunately despite multiple infection prevention and control measures being put in place, many hospitals in the UK experienced high numbers of hospital onset COVID-19 cases.
The sheer numbers of infections occurring in a short space of time within the hospital environment means that it is often impossible to work out “who infected whom” from traditional contact tracing alone. In the case of healthcare workers, it is also very difficult to determine whether infections were acquired at home or at work during periods of high community SARS-CoV-2 prevalence. However, the unprecedented scale of genomic sequencing performed during this pandemic through projects such as the COVID-19 Genomics UK Consortium, have opened up new opportunities to understand viral transmission dynamics within hospitals.

In our recent paper, published in Nature Communications, we use genomic data in combination with epidemiological information to model the spread of SARS-CoV-2 in a large UK National Health Service Hospital Trust. A common issue faced when trying to reconstruct transmission chains of SARS-CoV-2 using genetic data alone is that the virus mutates too slowly to introduce genetic variation over the time course of a single infection. To overcome this limitation, we combine genetic sequence with knowledge of symptom onset dates and hospital location data for patients and staff to build more accurate models of SARS-CoV-2 transmission.
By applying this methodology we have been able to understand several key aspects driving hospital transmission which have been used to improve current infection control practice. The first finding is that not all hospital wards are equally likely to see SARS-CoV-2 transmission. We found hotspots within the hospital with approximately 10% of wards accounting for 50% of all transmission. Interestingly, the top ten hotspots changed from the first to the second wave of the UK epidemic, which likely represents the dynamic and complex environment of an NHS hospital adapting to multiple pressures.
Over time, who infected whom within the hospital also changed significantly. Early on during the first wave of the UK epidemic in 2020, staff to staff transmission accounted for around a third of all infections occurring within the hospital environment, dropping to around 1 in 6 in the second wave (late 2020 to early 2021). This may have been due to the variety of infection control measures introduced, such as universal wearing of face masks even in areas where only staff were present. Conversely, patient to patient transmission increased from approximately a quarter of infections within the hospital in wave 1 to around half of all transmissions in wave 2.

One concern has been that hospital outbreaks may be characterised by large ‘super-spreader’ events. In contrast, our results show that most hospital onset cases resulted in no, or minimal, onward transmission. Around a half of cases had no associated secondary infections and approximately 95% of cases transmitted to less than or equal to 2 people.
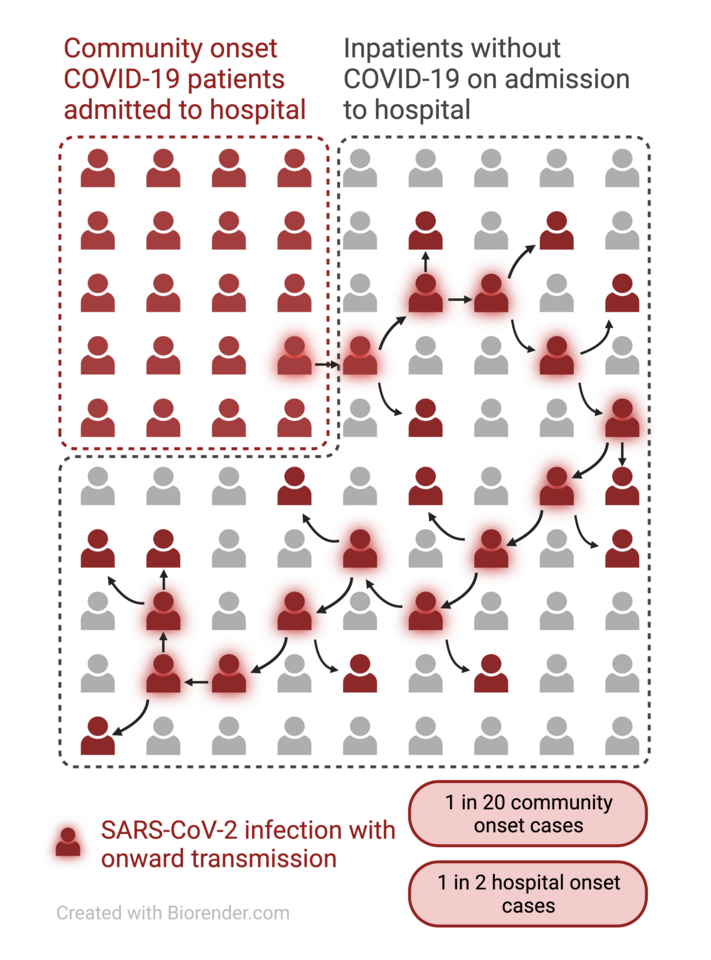
Our most significant and likely practice changing result is that the probability of onward transmission is markedly different for community onset and hospital onset cases. Cases that are acquired within the hospital result in onward transmission around 50% of the time, compared to 5% of the time for cases which are acquired in the community and are subsequently admitted to hospital. Several factors may explain this observation. Patients who already come into hospital with a diagnosis of COVID-19 are likely isolated more quickly. They may also be later in their illness when people tend to be less infectious. Our findings suggest that hospital transmission is driven by patients who acquire SARS-CoV-2 in hospital and then transmit on before identification and isolation. We believe that earlier identification and isolation of hospital acquired cases can help reduce the size and impact of hospital outbreaks. More frequent testing of admitted patients with tools such as point-of-care tests which provide rapid results may be required to achieve this.

Hospital outbreaks of COVID-19 are likely to be an ongoing problem for years to come. We show that genomic sequencing combined with traditional epidemiological data can be used to understand the complex transmission chains which occur within a hospital. This can help improve the safety of patients and hospital staff alike. Both genome sequencing and data science technologies have progressed considerably in the last decade and we now need to ensure that all hospitals have access to these tools. Integrated and automated informatics to make sense of complex systems such as viral transmission within the hospital environment are required to have a real-time impact, not just for SARS-CoV-2, but for other viruses causing hospital outbreaks such as influenza and norovirus. Striving to achieve this paradigm shift in infection control practice more widely should be the focus of ambitious planning and strategy at global, national and institutional level in order to provide the very best care for our patients.
Our publication can be accessed in the following Open Access link:







Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in