Imagine at age 20 you learn that you suffer from a chronic disease. You will never be free of it, it might cause you pain, weight loss or inability to control when you need to use the bathroom. The disease course is impossible for your doctor to predict, and you probably need to take medication for the rest of your life or even undergo surgery and possibly be left with a stoma at some point in the near or far future. You probably have to take many sick days from school or work, and you could face unemployment or work disability as a result. This is the reality for many patients, who are diagnosed with inflammatory bowel disease (IBD).
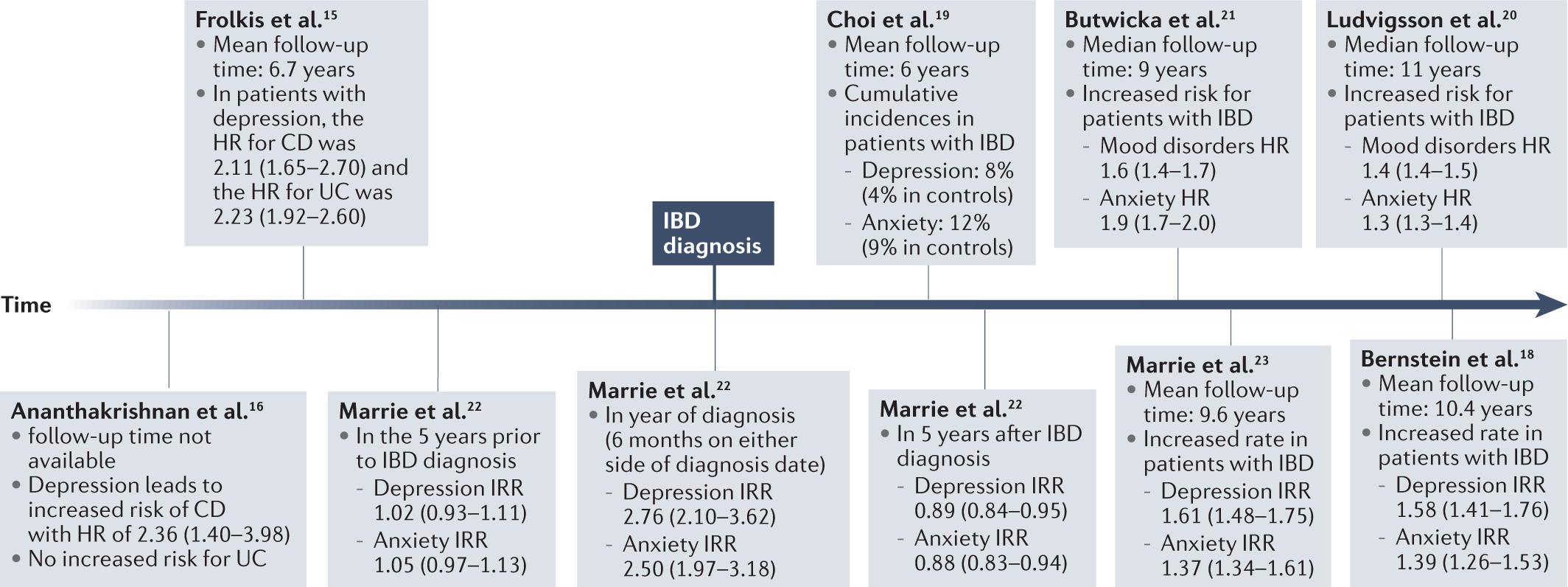
With this outlook in mind, it is not hard to imagine that patients with IBD could struggle with their mental health and even develop depression or anxiety. We know that patients with IBD are more likely than their peers to have depression and anxiety. However, it is still unclear to what extent these diseases occur together and in what sequence they arise.
In recent years, there has been a growing insight into the communication between the gut and the brain through the so-called "gut-brain axis”, which involves signaling thought the autonomic nervous system, immune system, neuroendocrine system, hypothalamic-pituitary-adrenal axis, and metabolites. This intricate system might contribute to the development of depression and anxiety in patients with IBD, and it could communicate in the other direction and contribute to development or worsening of IBD in individuals with depression or anxiety.
In this review now out in Nature Reviews Gastroenterology & Hepatology, we explore the connection between IBD, depression and anxiety. We summarize the epidemiology of the co-occurrence, including the temporal relationship between the diseases and the influence of psychological stress on IBD onset and disease course. We discuss the possible biological mechanisms that link the diseases and the effect of antidepressants and psychological interventions on IBD and of IBD medication on depression and anxiety.
This review establishes that depression and anxiety are major comorbidities in IBD patients, affecting somewhere between 15%-35% of IBD patients. The relationship between the diseases seems to be bi-directional with depression and anxiety being more prevalent in IBD patients compared with individuals without IBD both before and after IBD diagnosis. Further, the available literature suggests that IBD patients with depression or anxiety are at an increased risk for a more active IBD disease course. From our review of biological mechanisms, it is likely that depression and anxiety occur in patients with IBD not simply due to the burden of living with a chronic disease but also because of this bidirectional signaling between the gut and the brain. Finally, antidepressants might be able to affect IBD disease course, either directly or through improvement of depression or anxiety.
Unfortunately, many IBD patients do not receive optimal care for their co-occurring depression and anxiety. In most health care systems, medical specialties are divided into separate clinics with little or no communication or collaboration. Obviously, gastroenterologists treating IBD patients are not and should not be experts in psychiatry or psychology. However, patients with IBD would benefit from an increased awareness on their mental health. IBD clinics could offer screenings for psychiatric diseases at regular intervals and especially at the time of IBD diagnosis. There is a need for comprehensive care for IBD patients, and IBD clinicians should ideally work closely with mental health providers or at the very least be able to refer their patients to quick psychological or psychiatric evaluation and treatment.
In conclusion, depression and anxiety are common and important comorbidities in patients with IBD. The diseases seem to influence and possibly worsen each other, and IBD clinicians should be aware of the mental health of their patients with IBD. It is important to provide appropriate and timely management of depression and anxiety along with the management of IBD to ensure a better result of treatment as well as improved quality of life.



Please sign in or register for FREE
If you are a registered user on Research Communities by Springer Nature, please sign in